By Nina Lemieux, Natalie Weston, John Harman, Faiz Baqai, Umer Khan
Empathize, define, ideate, prototype, and test. In January 2020, a group of students from Dell Medical School at The University of Texas at Austin enrolled in Introduction to Biomedical Device Design: an elective course where medical students led teams of undergraduates to learn and execute this five-step design process. Interdisciplinary teams employ this pathway to define problems, identify target populations, challenge existing ways of thinking, and ultimately develop and refine a potential solution. Though each team worked independently on their respective projects, the goal for all students in this course was to develop an understanding of this often asynchronous and iterative process by designing a medical device to solve a problem of their choosing. In March 2020, that goal shifted. Wanting to serve on the front lines of the COVID-19 pandemic but not yet having the clinical skills necessary to do so, students in the course decided to work on designing devices that could immediately be utilized. Though the pandemic scattered team members across the nation and eliminated student access to lab equipment, two teams successfully built working prototypes of their devices. This paper details how these teams successfully navigated the process of design thinking under the limitations of reduced resources and social distancing guidelines to produce tools to improve emergency ventilation and telehealth.
Project 1: Emergency Ventilation
Video 1: Pneumatic Ventilator in Action

In March of 2020, a surge in COVID-19 patients requiring mechanical ventilation resulted in regional ventilator shortages around the globe. Researchers sought to address the shortages by developing designs that could be rapidly constructed and distributed to areas in need. It was in this setting that we returned to our Introduction to Biomedical Device Design course to tackle the challenges of healthcare during a global pandemic.
As a team of first-year medical students and undergraduates, none of us had ever seen, let alone operated, an actual ventilator when we began our design process. Our first objective was to determine the necessary capabilities of an emergency ventilator. We arranged a short Zoom consultation with UT’s ventilator design team and then independently reviewed open-source designs shared by other institutions. Our team concluded an emergency ventilator should be able to monitor pressure and adjust tidal volume, inspiratory/expiratory ratio, respiratory rate, and positive end-expiratory pressure (PEEP).

Next, our team assessed the pros and cons of the other ongoing emergency ventilator projects. We discovered that most other designs used a motorized device to squeeze an Ambu bag. Using an Ambu bag as the centerpiece of such a device offers a clear advantage in an emergency scenario due to its availability. However, Ambu bags have several limitations including difficulty in accurately regulating tidal volume. Additionally, some of the mechanical contraptions being designed to operate the Ambu bag required specialized or 3D-printed parts, and many used PLC boards requiring programming. We saw this as an opportunity to come up with an equally reliable design that did not require any special parts. We wanted something that was easy to build, operate, maintain, and source, requiring only a few parts. In the setting of a global pandemic, a simple ventilator design like ours would provide a solution for both areas of remote access and urban hospitals made resource-poor by global supply shortages.
What is truly amazing about working with an interdisciplinary team is that a single problem can be viewed through a multitude of lenses. The idea to use pressurized air to power our ventilator arose from the experience of one of our team members who once worked as an engineer on ships. He found that shipboard automation systems controlled by compressed air were reliable and easy to operate. With input from medical students on the team, we also knew that compressed air supplies, referred to as medical air or instrument/surgical air, already exist in hospitals. This air is highly filtered and dried in hospital settings, making it ideal for operating precision tools and equipment.

Our initial sketches were as simple as seen in Fig. 1. To demonstrate the basic idea of pneumatically controlled ventilation, we used an air compressor to manipulate a blood pressure cuff wrapped around an Ambu bag (Fig. 2). Basic control circuits and regulating valves, similar to what one might find in shipboard propulsion plants, were incorporated into our design to provide automation. By the end of the course, we had a unique and theoretically sound blueprint for a pneumatic ventilator. However, we didn’t stop there. Through a series of iterative adaptations using only readily available components, we were able to design and build a fully functional pneumatic ventilator (Fig. 3, Video 1).
Project 2: Muscle Strength Assessment in Telehealth
The second project addressing biomedical device design within the context of COVID-19 focused on the growing utilization of telehealth. Due to limitations of in-person visits, physicians sought creative ways to conduct a physical exam virtually. When considering the head-to-toe exam and researching existing products, we found that vital signs, parts of the neuro exam, and basic range of motion could be assessed via telehealth with minimal to no equipment. However, when our team observed a telehealth call between a Physical Medicine and Rehabilitation physician and his patient, our team recognized that the virtual assessment of strength was sorely lacking.
Traditionally, physicians, nurses, physical therapists, and occupational therapists assess muscle strength using the manual muscle test (MMT), which grades strength on a scale of 0–5 (Table 1). However, in practice, the MMT lacks inter-rater reliability and poorly distinguishes the gradient between those barely able to move against gravity and those almost back to full strength—a clinically essential distinction for patients who are recovering from an injury or who suffer from a degenerative condition. When designing our telehealth product, we sought to create a cost-effective tool that could be used virtually to provide a more accurate and quantified measure of strength.
| Grade | Description |
|---|---|
| Grade 0 | No muscle contraction can be felt in the gravity-eliminated position. |
| Grade 1 | Flickering muscle contraction in the gravity-free position. |
| Grade 2 | Patient has complete range of motion in the gravity-free position. |
| Grade 3 | Patient has complete range of motion against gravity. |
| Grade 4 | Patient has complete range of motion against gravity + some resistance. |
| Grade 5 | Patient has complete range of motion against gravity + full resistance. |
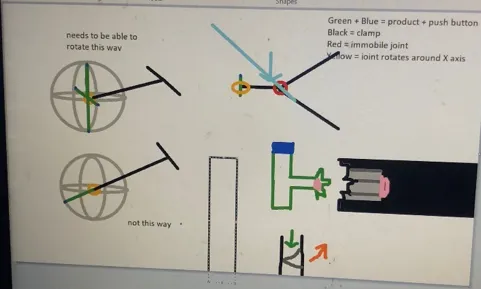
Our team consisted of two medical students and two exercise science students, geographically separated due to virtual learning during COVID-19. The typical hands-on design process was shifted as we experimented with ways to wireframe without in-person feedback. Our first steps included getting input from experts in neurology, physical therapy, and physical medicine and rehabilitation. We learned about the physical limitations of many patients who would need a strength assessment device and drew an initial design on AWW App, a free, web-based group whiteboard.
Our initial design required the compression of a button on the end of a rod, which would have a small Bluetooth scale inside. However, stabilizing the rod proved difficult, and one of our medical students noted the cost required to integrate the Bluetooth scale. An exercise science teammate pointed out the possibility of using tension to measure strength instead using standard gym equipment as an existing reference point.

Unable to have in-person meetings, we continually shared rough sketches of design modifications via Slack (Fig. 3). This proved beneficial because it allowed for real-time troubleshooting not just at a single weekly meeting, but whenever someone had a new insight to share. We also utilized FaceTime and household objects to clarify ideas in three dimensions. The spontaneous nature of our COVID-adapted prototyping allowed for an accelerated design process that culminated in a working prototype in just under three weeks (Fig. 4).
An important consideration in our design process was affordability. While some physical therapy practices use dynamometers, these are too expensive for individuals to buy for use in their homes. Adapting our sketches to building from readily available products—including a trigger-action clamp, a luggage scale, and a hook-and loop-strap—our team produced a functional device that could be produced for less than $8 (Fig. 5). While our final product would include an aesthetic plastic cover, our expected consumer cost would be less than $20.

Final Thoughts
Though the limitations of designing medical devices within the context of a global pandemic posed significant challenges, our teams were able to successfully use these restrictions to inspire innovation. While our teams eagerly anticipate the opportunity to test and refine our designs further in real-world settings when allowed by social distancing, these projects have demonstrated that the five basic tenets of design—to empathize, define, ideate, prototype, and test—apply even in unprecedented circumstances.
Read more from the Journal of Design and Creative Technologies

