Improving Patient and Provider Communication in Congenital Heart Disease Care
Challenge
How might we address fragmented care and improve patient, caretaker, and provider experiences within the Dell Children’s Congenital Heart Disease Clinic?
Context
Congenital heart disease (CHD) represents a complex umbrella of diagnoses requiring extensive, coordinated care. Children diagnosed with CHD often experience lengthy hospital stays and care plans that involve numerous specialists, including physicians, nurses, social workers, and psychologists. Their families must navigate new, unexpected realities, while balancing complex information and evolving emotional challenges.
The large care teams involved in each case often experience communication barriers, particularly between medical and psychosocial teams. These gaps in communication create friction, leading to less effective care and increased confusion for families already struggling to manage the complexities of their child’s condition. Families often feel overwhelmed by the information provided and may have difficulty engaging fully with their child’s care journey.

Approach
The project team, drawing on a previous research initiative called the Corage Project, used ethnographic research to observe clinical workflows and identify areas where design interventions could improve both the patient and provider experience. Through direct observation at Dell Children’s and collaboration with the care teams, the team identified key pain points in communication and care coordination. Their human-centered approach focused on creating solutions addressing patient-provider and provider-provider interactions.
Key activities included:
- Journey mapping to understand the patient experience from prenatal diagnosis through adulthood
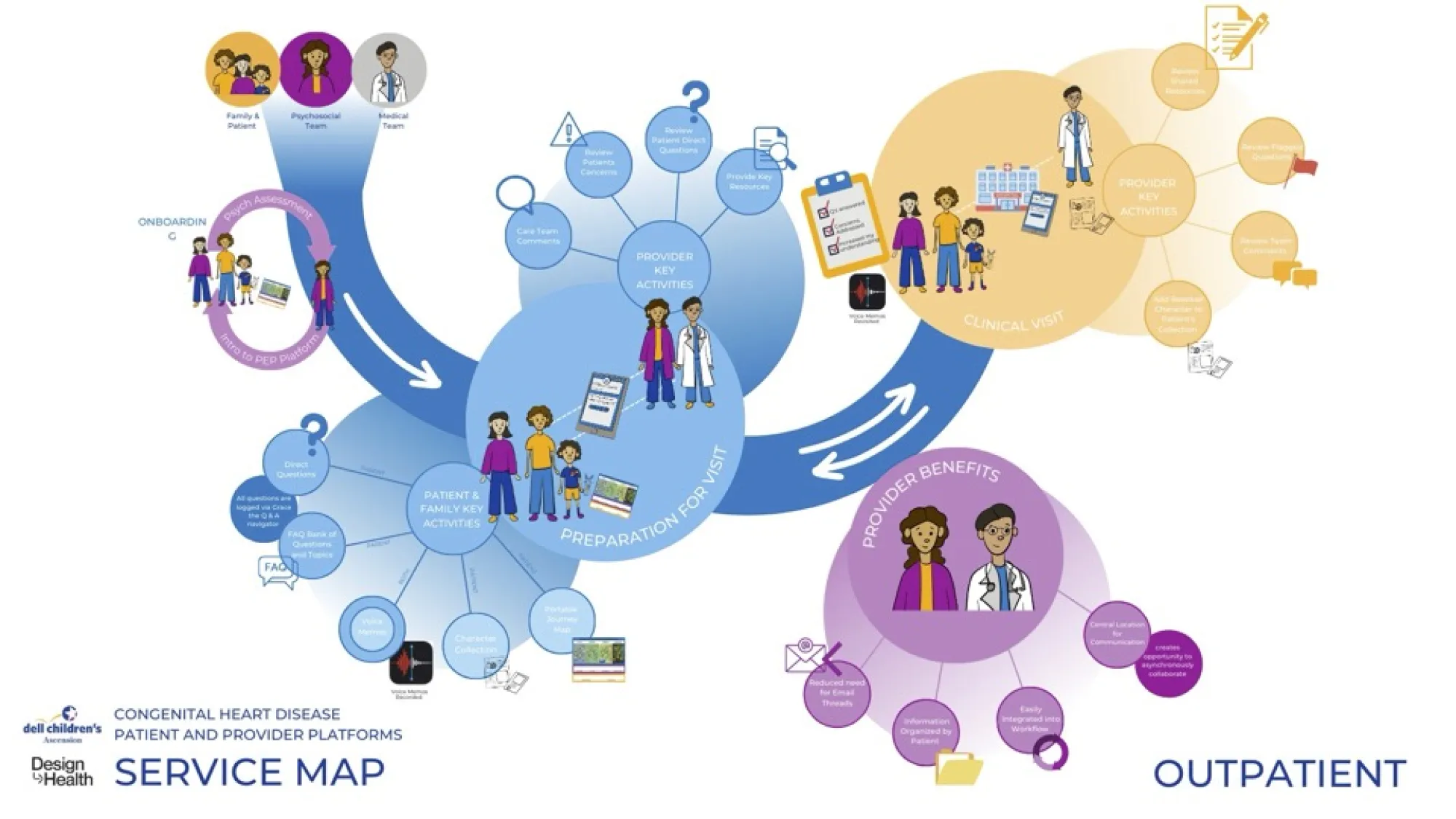
- Initial designs of a digital platform aimed at improving communication between the medical and psychosocial teams and streamlining information delivery to families
- Ideation and prototyping of over 100 concepts, eventually focusing on increasing teamwork among providers and improving families’ understanding of their child’s care

Insights
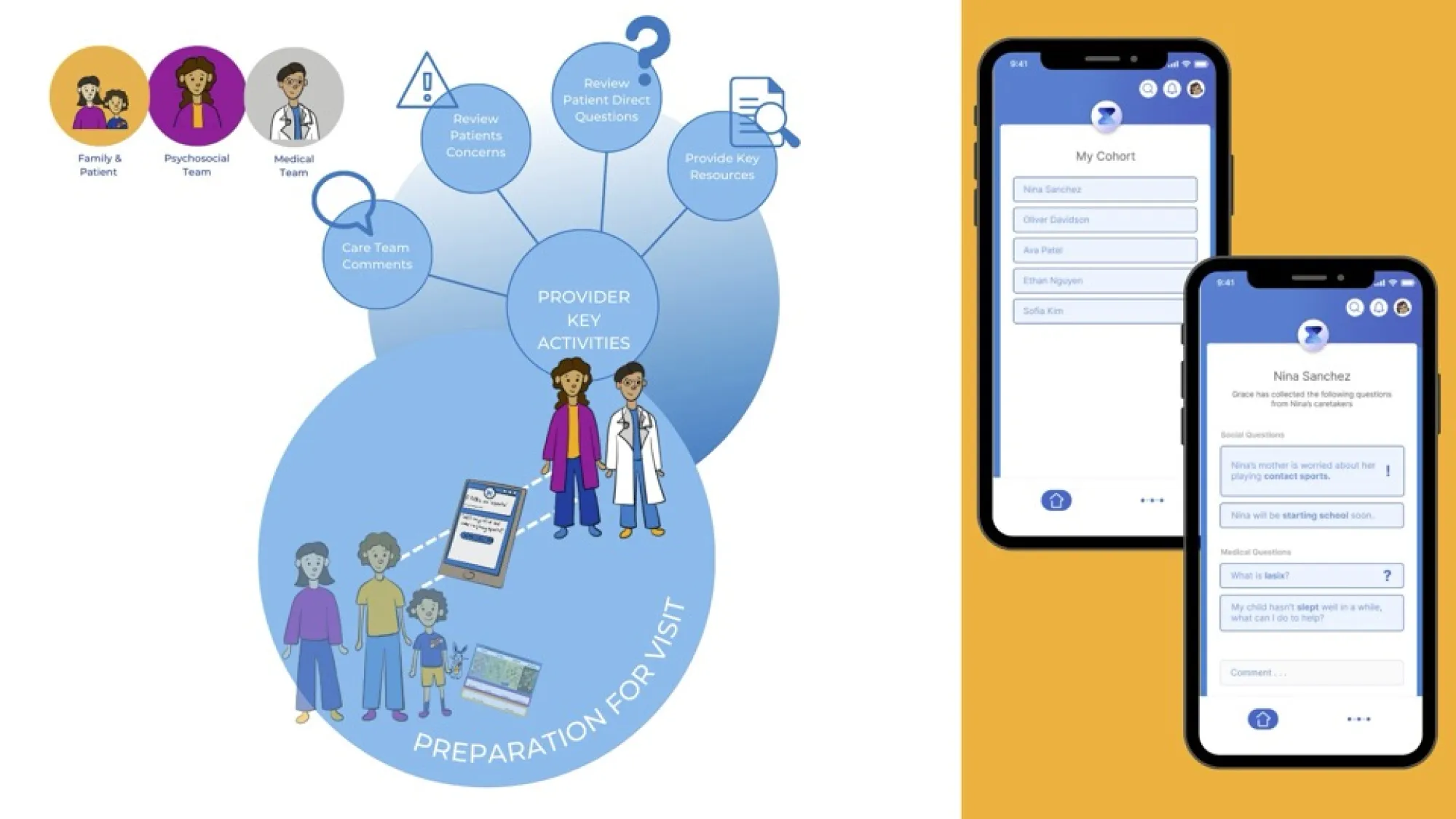
- Provider Communication: Miscommunication between medical and psychosocial teams creates unproductive friction in patient care. Standardizing the interaction between these teams was identified as a critical area for improvement.
- Family Confusion: Families are often left confused by the volume and complexity of the information provided during clinical visits. They frequently struggle to recall key details or ask important questions during the limited time they have with providers.
- Ethnographic Research Impact: Spending significant time shadowing the clinical team and observing patient interactions provided essential insights into the daily challenges faced by both families and providers, leading to better-aligned design solutions.
Solutions
The comprehensive patient experience platform incorporates both digital and physical tools to support care coordination and communication, achieving the following outcomes:
- Improved Communication: The platform enables better provider-to-provider communication, particularly between medical and psychosocial teams, ensuring that critical patient information is shared effectively and flagged for attention during clinical visits.
- Enhanced Family Engagement: A patient-facing portal allows families to ask questions, access resources, and prepare for visits more effectively. The introduction of a FAQ feature, along with a virtual assistant named “Grace,” will help streamline common concerns, making clinical interactions more efficient and meaningful.
- Positive Reception from Clinicians: More than 50 clinicians provided early feedback on the platform, expressing strong support for its potential to improve patient care. In a future development phase, the proposal would need to ensure HIPAA compliance and that the platform remained supplementary to, rather than a replacement for, in-person communication. Overall, the goal is to integrate these tools into the existing healthcare system to ensure better patient outcomes.






Learn More
Find out more about Dell Children’s Medical Center.
Design Team
Shontá Bradford
Mara Fock
Emily McCalley
Claire Moreau
Sanjana Nagaraja
Ayesha Rahman
Veronica Remmert
Jewel Thompson-Adiuku
Brooke Upchurch
Project Summary
To improve communication and care coordination for children with congenital heart disease, students partnered with Dell Children’s Medical Center to design a patient experience platform. Grounded in ethnographic research, their solutions supported collaboration between medical and psychosocial teams and empowered families through digital tools—easing confusion, enhancing preparation, and improving outcomes across the care journey.
Project Contributors
Dell Children’s Medical Center

